A Pilot Study using Vesicare™ (Solifenacin) in the Treatment of Urinary Incontinence after Radical Prostatectomy
Lead Researcher: Thomas Ahlering, MD
Study Abstract
Our original published finding suggested that ‘Detrusor Muscle’ instability results in excess contractions of the urinary bladder (‘urgency to urinate’), and can result in the feeling of needing to urinate more frequently. Consistent with this hypothesis of detrusor muscle instability, men with preoperative complaints of urgency, frequency and bother were at greater postoperative risk of incontinence. We proposed that a transient bladder muscle contraction overcomes the external urinary sphincter and resulting in the patient dribbling urine. Our hypothesis is that by treating the bladder muscle instability, we may expect improved postoperative continence and improved quality of life in patients after undergoing radical prostatectomy surgery.
We tested this hypothesis in a small pilot study of Vesicare subjects and a well matched control group; both had moderate to severe urinary symptoms preoperatively and both groups had endo-rectal hypothermia during surgery. We wanted to see if Vesicare reduced the time to pad free status. Remarkably in this trial group of 13 men there was a 50% reduction in the time to pad-free status. In the Vesicare group, all men achieved pad free status by 50 days (Kaplan Meier, Log-rank, p=.012, Wilcoxon, p= .022), while in the control group, 11/27 (41%) took longer than this to be pad-free. However in this initial study 3/13 (23%) stopped the med early and due to irritating side effects such as constipation and nausea within the first 2 weeks (57%). Our initial study supports that Vesicare, as an additive therapy for hypothermia, is synergistic for an earlier return to pad-free continence. In our view, a more effective study would investigate only men using one or more pads/day one week after catheter removal subsequent to robotic prostatectomy. This postoperative delay may reduce early side effects (e.g. tolerance of dry mouth, constipation) after radical prostatectomy and more effectively treat incontinent specific patients.
Introduction
Our publication1 on post-robotic prostatectomy urinary continence provided the basis for our hypothesis. We (and others) had seen two groups of men who were pad free following RP; one group (30-40%) indicated they never leaked “perfect” and the other did not wear pads but experienced occasional dribbling (60-70% “imperfect”). We asked “was the difference between the perfect and imperfect the result of a surgical issue or something the patient brought to the table.” We evaluated a host of peri-operative factors and baseline patient characteristics. We found that the “imperfect” group’s baseline characteristics demonstrated statistically older men who had higher bother scores, small voided volumes, and higher American Urological Association (AUA) symptom scores compared to the “perfect” group. Postoperatively, the “imperfect” group took longer to achieve a pad-free status, had higher AUA symptom scores, higher bother scores, and smaller voided volumes.
A consequence of robotic radical prostatectomy is a standardizing effect. In our experience, factors such as operative time, blood loss, and hospital stay have been notably consistent. In our minds, a central issue is that urinary leakage is a consequence of individual patient variables and not a consequence of a technical “mistakes”. Our findings strongly suggest that underlying detrusor instability was the logical etiology that would account for urinary leakage, irritative symptoms, and prolonged time to complete pad-free continence. Leach et al 2 studied 215 men urodynamically with post-prostatectomy incontinence and found 57% had detrusor instability as a major component of incontinence and 15% as the sole cause. Chao et al 3 found 43% of post-prostatectomy patients had detrusor instability or decreased compliance; however, this was the sole cause of incontinence in only 4%. A detrusor contraction may transiently overcome the urinary sphincter resistance and result in the dribbling of urine. Since detrusor instability occurs in approximately 75% of patients with benign prostatic hyperplasia (BPH), it follows logically this may account for the prolonged intervals to reach pad free status, and urinary leakage postoperatively.
Our findings in Rodriguez et al1 supported the inherently logical principle that pre-existing urinary voiding symptoms persist and affect urinary control in obtaining pad-free continence. We believe men with detrusor instability and decreased bladder compliance are potential candidates for early intervention with anticholinergic therapy (e.g. solifenacin, Vesicare) for return of pad-free and drip-free continence. Our hypothesis is that this therapy will decrease the time to pad free continence, and pad-free and drip-free continence, and significantly benefit in quality of life for men in continence after radical prostatectomy.
Solifenacin Pilot Study Results
We have completed an initial pilot study designed as a clinical trial of men who had robotic radical prostatectomy surgery for recovery of their urinary function. The men used the FDA approved medication ‘Vesicare’ for overactive bladder (OAB) symptoms to reduce irritating urinary symptoms of frequency and urgency after surgery. The intent was to also reduce urinary incontinence and discomfort which usually follows surgery persisting through many months. These men were asked to take a 5 mg daily dose of Vesicare for 3 months, and could discontinue the medication after 1 month, if they have attained pad-free continence.
Efficacy
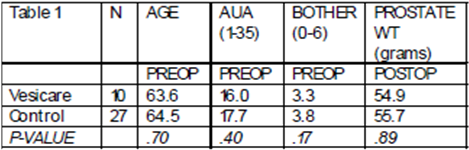
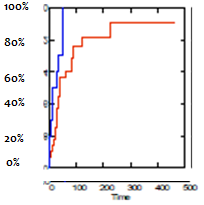
Table 1 demonstrates that the Vesicare and control groups are well matched, and both have moderate to severe urinary symptoms pre operatively. Vesicare reduced the mean time to pad free status by 50%. A Kaplan Meier graph of time to % pad free urinary continence versus time in days ( below right-Vesicare [blue], control [red] lines) shows this significant difference in earlier continence return in men, (Log-rank, p=.012, Wilcoxon, p= .022). In the Vesicare group, all men achieved pad free status by 50 days, while in the control group, 11/27 took longer than this to be pad-free. AUA scores dropped from PreOP average 15.6 to 8.8 at 3 months, and this was similar for Bother scores (pre 3.2 to 1.5 at 3M). These initial results are encouraging in this small patient sample.
 |
 |
|---|
Compliance and Side Effects
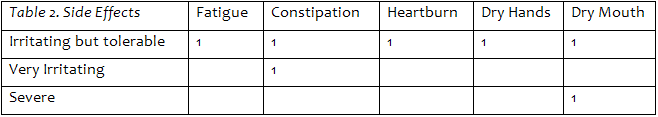
The use of Vesicare immediately after Radical Prostatectomy to specifically reduce the time to pad-free status is novel. In the pilot study 13 men were consented to Vesicare and matched with 27 control men who were not on Vesicare. Three men withdrew from the study early; 2 because they became pad free and regained urinary control quickly in a few days, and believed Vesicare would have no further impact on continence. One subject discontinued due to nausea. Table 2 lists the moderate side effect(s) for each of the 10 study patients; minor side effects are not included. Seven men reported irritating or greater side effects, two had pronounced symptoms. We note that 4 of these 7 men had these symptoms only within the first 2 weeks after catheter removal, when they are most vulnerable after surgery. We found initial findings of 1.Compliance issues of 3/13 (23%), and 2. Early irritating to severe side effects within the first 2 weeks (57%).
The small numbers of Vesicare patients did not impact our findings, and were dropped out of our published hypothermia analysis. However in this small Vesicare pilot study, a significant benefit developed for those men also using the medication. At this time, we only offer hypothermic radical prostatectomy to our patients due to its significant reduction in time of urinary pad usage, across all ages 4-5 , and preliminary evidence in improving sexual function in men with larger prostates.
A recent study by Van Kampen et al 6 concludes that men with increased amount of urine loss as early as the 1st day is predictive of delayed return of pad free continence, and we have noted the same trend in our patients. We believe that utilizing Vesicare now only in cases of confirmed postoperative incontinence, will achieve three goals: 1. Accurately target the men with copious urine leakage needing treatment, 2. Increase compliance with the study requirements with an extra one week recovery window in these incontinence postoperative, and 3. Reduce the frequency of irritating to severe side effects for better patient acceptance. This new study will assess the statistical requirements for the number of subjects needed for a fully ‘powered’ multi-institutional randomized prospective study to fully evaluate whether medications such as solifenacin significantly improve patients’ quality of urinary life and improve postoperative urinary incontinence after surgery.
Summary
Our initial study supports that Vesicare, as an additive therapy for hypothermia, is synergistic for an earlier return to pad-free continence, but caution is advised as nearly 25% of our subjects discontinued Vesicare before the initial 30 day trial minimum, and 57% experience irritating side effects within the initial fortnight when treatment was begun immediately within one week after surgery.
References
1. Rodriguez, E., Skarecky DW, Ahlering TE, ‘Perfect’ Continence Outcomes after Laparoscopic Radical Prostatectomy. Urology 67(4): 785-788 April 2006.
2. Leach GE, Trockman B, Wong A, et al, Post prostatectomy incontinence, urodynamic findings and treatment outcomes. J. Urology 155: 1256-1259, 1996.
3. Chao R and Mayo ME, Incontinence after radical prostatectomy: Detrusor or sphincter causes. J. Urology 154: 16-18, 1995.
4. Finley D, Osann K, Skarecky DW, Ahlering TE, Hypothermic nerve sparing radical prostatectomy: rationale, feasibility, and impact of early continence. Urology 73(4): 691-696, 2009.
5. Finley D, Chang A, Santos, R, Skarecky DW, Ahlering TE, Hypothermic Radical Prostatectomy: Impact on Continence J Endourology 23 (9): 1443-1450, 2009.
6. Van Kampen M, De Weerdt GW, Van Poppel H, An easy prediction of urinary incontinence duration after retropubic radical prostatectomy based on urine loss the first day after catheter withdrawal. J Urology 181: 2461-2646, 2009.
